At CHI Health, we are committed to support women with or at risk for diabetes. In partnership with your provider, our diabetes education team of nurses and dietitians provide a variety of outpatient diabetes education and support from pre-pregnancy through pregnancy into the postpartum period
What is Gestational Diabetes?
Gestational diabetes is a type of diabetes that happens during pregnancy. Unlike type 1 diabetes, gestational diabetes is not caused by having too little insulin. Instead a hormone made by your placenta keeps your body from using the insulin as it should. This is called insulin resistance. Blood sugar (glucose) then builds up in your blood instead of being absorbed by the cells in your body.
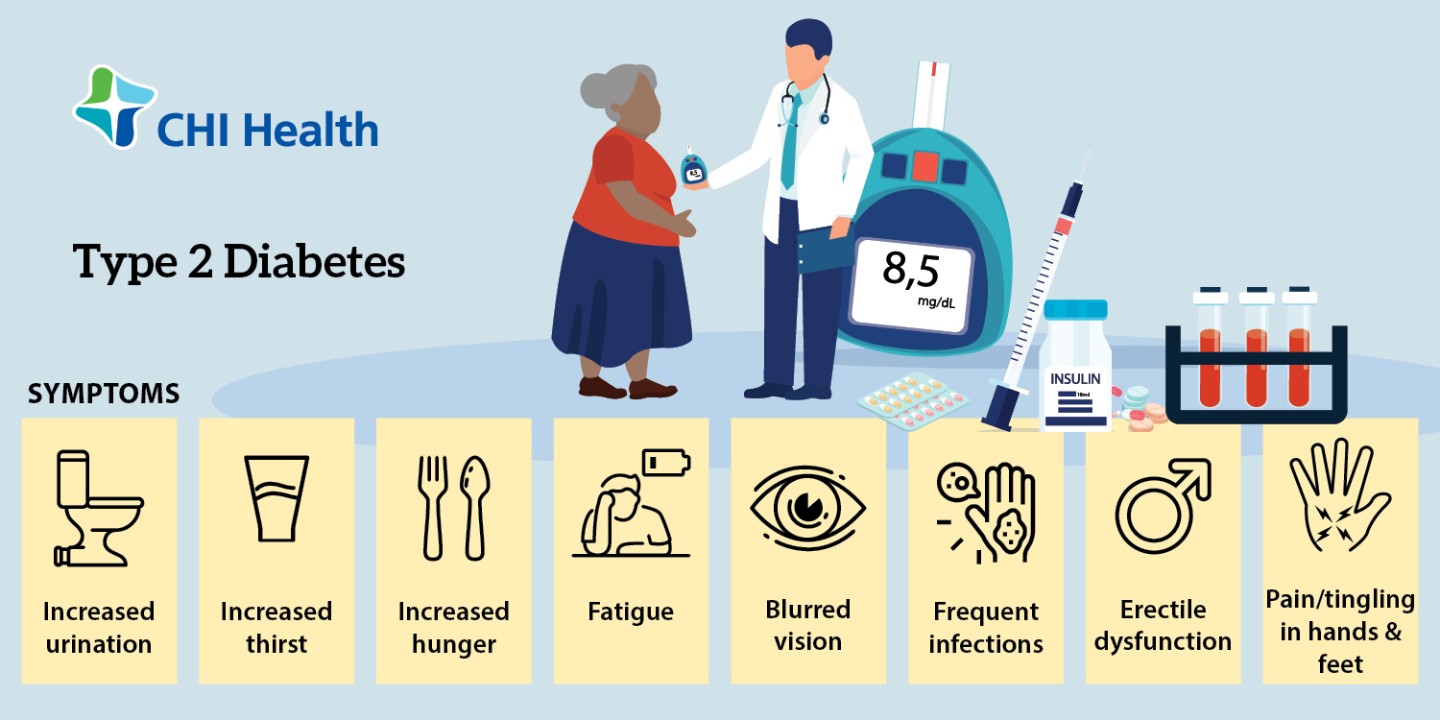
What are the symptoms of gestational diabetes?
Gestational diabetes does not cause any symptoms. That’s why it’s important to get tested for it if you are at high risk. If your blood sugar levels are very high, you may have these symptoms:
- You urinate more than normal
- You are hungrier or thirstier than normal.
- You have blurred vision
- You have nausea and vomiting
- You lose weight even though you are hungrier
How is gestational diabetes diagnosed?
You should be tested for gestational diabetes in your 24th to 28th week of pregnancy. The American Diabetes Association also recommends that you be tested for type 2 diabetes if you have risk factors for this condition. This testing should be done at your first prenatal visit. Screening is done by these tests:
- One-hour glucose tolerance test. You drink a special beverage high in sugar. One hour later, the healthcare provider measures your blood sugar (glucose) levels. If your levels are higher than a certain level, this is considered an abnormal result.
- Three-hour glucose tolerance test. If the 1-hour test is abnormal, you will have a second glucose tolerance test done to confirm the diagnosis. You will drink another special beverage, but with more sugar. Your healthcare provider will measure your blood sugar levels 1 hour, 2 hours, and 3 hours later. You have gestational diabetes if at least two of the glucose measurements are higher than normal.
If you are diagnosed with gestational diabetes, you should get tested for diabetes 4 to 12 weeks after your baby is born. You should also get this screening at least every three years for the rest of your life.
What is the treatment for gestational diabetes?
Treatment for gestational diabetes focuses on keeping your blood sugar levels in the normal range. Treatment may include:
- Special diet. You should eat 5 servings of vegetables, fruits, low-fat or nonfat dairy products, and lean meats. Use liquid fats for cooking instead of solid fats. You should eat whole grains and avoid high-calorie snacks or sweet desserts.
- Exercise. You should do moderate exercise unless your healthcare provider tells you not to.
- Daily blood glucose monitoring. Your goal is to keep your blood sugar levels lower than 130mg/dL to 140mg/dL one hour after eating.
- Insulin injections. You may need these to control your blood sugar levels. Or you may need other medicines taken by mouth.
Our Gestational Diabetes Education program will assist you with your special diabetes management needs during pregnancy. The program consists of:
- Nutrition education including an individualized meal plan with one or more sessions with the registered dietitian.
- Self-management education including blood sugar monitoring, sick day care, target blood sugars, and physical activity.